When your lungs stop working and your heart is failing, there are not many options left. But one of the last lines of defense modern medicine has to offer is called ECMO, short for Extracorporeal Membrane Oxygenation. It is a complex and high-risk procedure, but it has saved countless lives in situations that seemed hopeless.
This is not a technology you hear about unless your life, or the life of someone you love, is suddenly in danger. But understanding how ECMO works, what it does to the human body, and what the risks are, can be the difference between panic and clarity in the worst moments of life.
What Exactly Is ECMO?
ECMO is a form of life support used in critical care units for patients whose heart or lungs (or both) are no longer able to function on their own.
The name might sound intimidating, but the concept is simple in theory: ECMO is a machine that takes over the function of the lungs and sometimes the heart. It oxygenates the blood and removes carbon dioxide outside the body, giving the organs a chance to rest and recover.
This therapy comes into play only when every other option has been exhausted. It goes far beyond a regular ventilator and is never considered a simple backup. Doctors rely on it as the last resort to keep a patient alive and stable while the body recovers or awaits a life‑saving transplant.
The Basic Mechanics: How ECMO Works
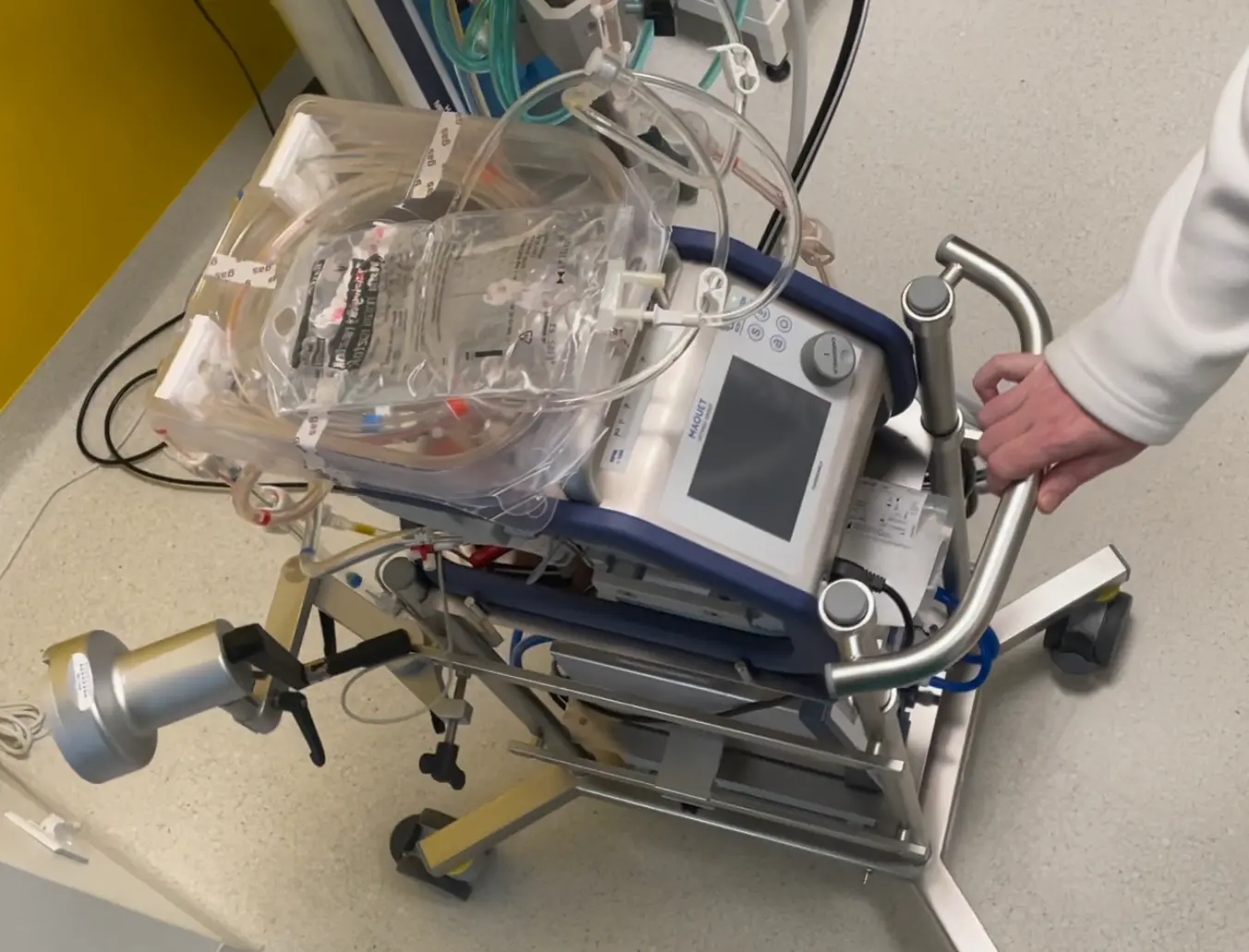
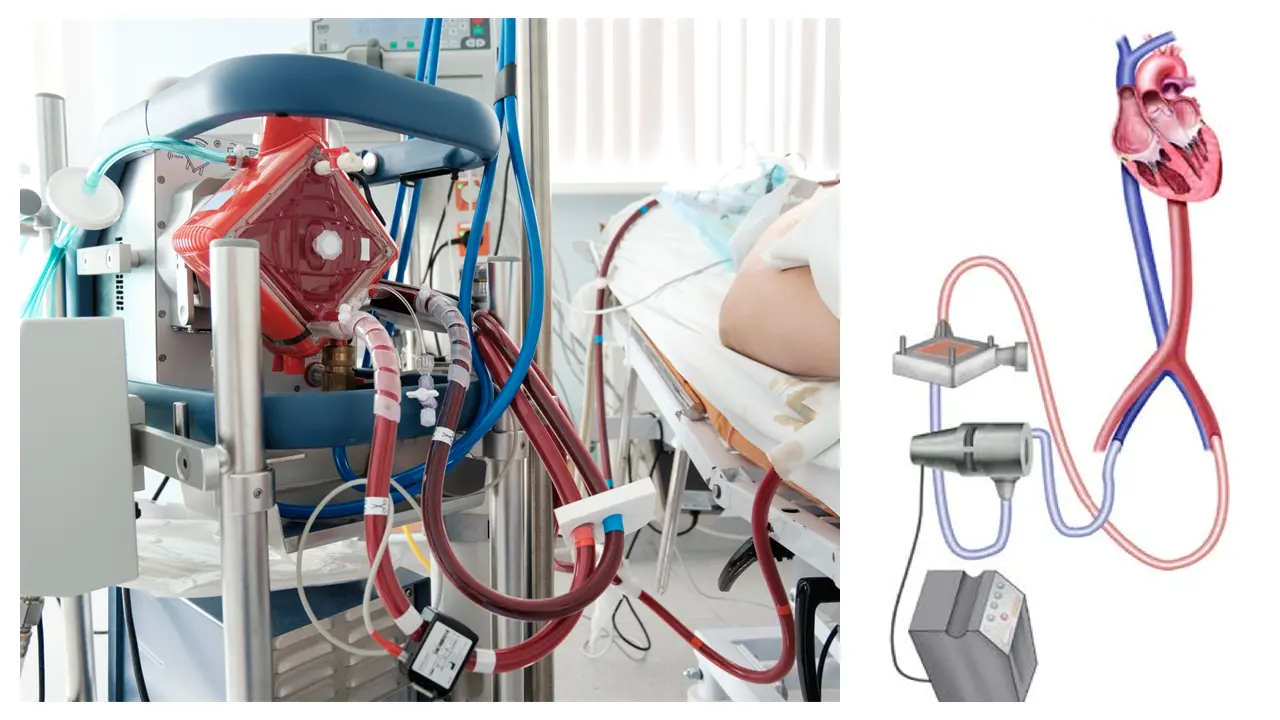
The ECMO machine is a highly advanced circuit of pumps, tubes, and an artificial lung. It involves inserting large cannulas (thick tubes) into major blood vessels, typically in the neck, chest, or groin.
Blood is drawn from the body, pumped through a membrane oxygenator, where it gets oxygen and loses carbon dioxide, and then returned to the body.
The oxygenator acts like a pair of artificial lungs. In some configurations, the machine also acts as a heart by circulating the blood for the patient.
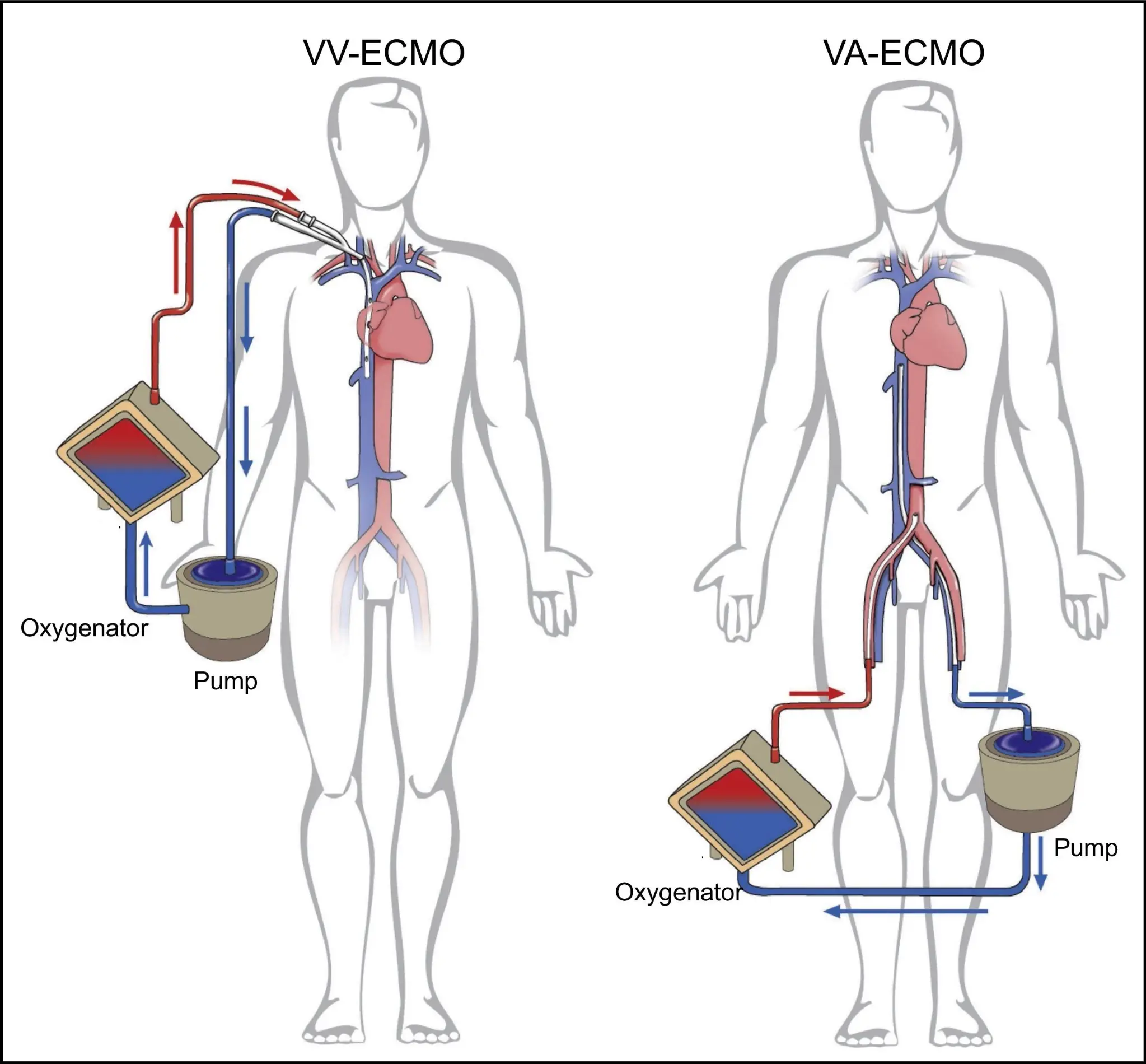
There are two primary types of ECMO:
1. Veno-Venous ECMO (VV-ECMO)
Used for patients whose lungs have failed, but whose heart is still functioning. Blood is drained from a vein, oxygenated, and returned to a vein. The heart continues to pump the oxygen-rich blood naturally.
This is often used in cases of:
- Severe pneumonia
- Acute respiratory distress syndrome (ARDS)
- COVID-19 complications
- Near-drowning or smoke inhalation
2. Veno-Arterial ECMO (VA-ECMO)
Used when both the lungs and heart are failing. Blood is drained from a vein and returned to an artery after oxygenation, essentially bypassing both organs.
This is used in:
- Cardiogenic shock
- Massive heart attack
- Cardiac arrest
- Post-surgical heart failure
When Is ECMO Used?
Doctors do not use ECMO lightly. It is expensive, invasive, and comes with significant risks. It is reserved for the sickest patients, usually those in intensive care who are not responding to conventional treatments.
Some common scenarios include:
- Severe respiratory failure where oxygen levels cannot be maintained even with a ventilator
- Refractory cardiac arrest where traditional resuscitation fails
- Bridge to transplant when a patient needs heart or lung transplantation and ECMO keeps them alive until a donor is found
- Septic shock or trauma where the body is overwhelmed and organs begin to shut down
In many hospitals, a special ECMO team decides if a patient qualifies for it. The criteria are strict, because the treatment is not always appropriate, especially if the chance of recovery is low.
What Does It Feel Like to Be on ECMO?
Patients on ECMO are usually deeply sedated or in a medically induced coma. Most are intubated and on a ventilator as well. The treatment is intense, and people on ECMO often require full organ support, including dialysis and blood pressure medications.
They cannot eat, speak, or move much. Family members are often the ones witnessing the process, which can be overwhelming. The machine is large, noisy, and surrounded by tubes and monitors. ICU nurses monitor the patient 24/7. It is a race against time, and every day on ECMO is filled with uncertainty.
How Long Can You Stay on ECMO?
The average time on ECMO is between 5 and 21 days, but some patients have survived after being on it for over 50 days. The duration depends on the condition being treated and how well the patient is responding. The longer someone is on ECMO, the higher the risk of complications.
ECMO is not meant to be permanent. It is a bridge, either to recovery, surgery, or a decision about end-of-life care.
Risks and Complications
Despite its life-saving potential, ECMO carries many risks:
- Bleeding: Because patients need blood thinners to prevent clots, bleeding (especially in the brain) is a serious risk.
- Infection: The cannulas go deep into the body and can become sources of infection.
- Stroke: Clots or air bubbles in the circuit can cause strokes.
- Organ failure: The stress of critical illness may lead to liver, kidney, or brain damage.
- Limb ischemia: In VA-ECMO, poor circulation may affect limbs, sometimes requiring amputation.
These risks are why ECMO is used only when absolutely necessary, and only in specialized hospitals with trained ECMO teams.

Success Rates and Recovery
Survival rates vary widely based on the underlying condition. According to data from the Extracorporeal Life Support Organization (ELSO):
- VV-ECMO survival is about 60 percent
- VA-ECMO survival is closer to 40 percent
Recovery does not end when ECMO is removed. Many patients spend weeks or months in rehab. Muscle loss, memory issues, and PTSD are common after long ICU stays. But for many, the alternative would have been certain death.
Innovations in ECMO
In recent years, ECMO has been adapted to smaller, more portable systems. It played a major role in saving patients during the COVID-19 pandemic, especially in younger individuals with otherwise healthy lungs that failed due to viral pneumonia.
Research is also underway on how to use ECMO during CPR, a method called ECPR, which could dramatically increase survival in cardiac arrest.
Some centers are even testing awake ECMO, where patients are conscious and breathing spontaneously while on the machine, which may improve long-term outcomes.
Quick Tips for Families and Caregivers
If you are supporting someone in the ICU and they are placed on ECMO, your days may be long and emotionally draining. You may need to stay close to the hospital for days or weeks.
Here are a few reliable platforms to book accommodation near hospitals:
- Book with Booking.com
- Compare on Kayak
- Find apartments via VRBO
- Check Expedia
- Use Agoda for hospital-area deals
And one more practical thing: hospital Wi-Fi is open and unprotected. If you are checking sensitive emails or doing anything private online, use a VPN to protect your data.
Recommended options:
- NordVPN – 77% off + 3 months free
- Surfshark – 87% off + 2 months free
- ExpressVPN – 73% off + 4 free months
They work even on hospital networks and take just one click to activate.
Final Thoughts
ECMO is one of the most advanced tools in modern intensive care. It is not a cure. It is a chance. It gives patients a fighting chance to recover when everything else has failed.
Doctors and nurses who work with ECMO patients witness both miracles and heartbreak. It is a field that requires incredible precision, patience, and compassion.
If someone you love ends up on ECMO, know that they are in the hands of some of the most skilled professionals in medicine.
And if you are that patient someday, know this – ECMO has saved lives that were once considered unsavable. Yours could be one of them.











